|
Celiac Disease Blood Tests and Biopsy--Diagnosing Celiac DiseaseCeliac disease blood tests are usually the first of two main steps in diagnosing celiac disease. Traditionally there was a panel of tests used known as the celiac panel. This panel included: -AGA IgA (anti-gliadin antibody) -AGA IgG (anti-gliadin antibody) -tTG IgA (anti-tissue transglutaminase) -Total IgA and sometimes -tTg EMA (anti-endomysium) Currently most doctors seem to rely on a single test, the tTG IGA or anti-tissue transglutaminase. The tTG test is highly specific for Celiac Disease and only rarely gives a false positive. It can not, however, rule out celiac as it will only pick up the antibody once it is in the bloodstream. You can still be susceptible to getting it, or have a mild enough case that the tTG levels are below the threshold of the test. The test will also be negative in a person with an IGA deficiency. 
This study shows the number of positive tTg test results on people who showed endoscopic evidence of celiac disease in various stages. It picked up almost every severe case, but a much smaller percentage (about 31%) of mild cases. Note: The study opens in a new window. If you have trouble opening it, you may need to hold down your control key while clicking to stop your popup blocker from blocking it. Journal of Clinical Gastroenterology
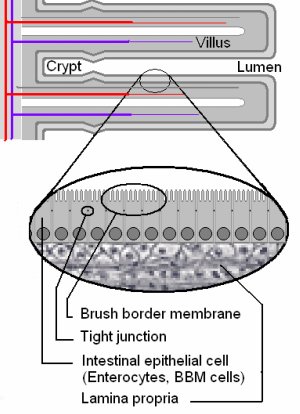
The Marsh system goes from 0 to 4, with 0 being normal and 4 being complete villous atrophy or a flat intestinal wall. If you have a 1 or a 2, you may have some changes in the epithelium where enterocytes have infiltrated or penetrated the tissue. This leads to "leaky gut", where the gliadin can enter the bloodstream. Also other food proteins can pass through and you may be reacting to many of these once they are able to enter the blood. At 3 you have partial or total villous atrophy plus the more permeable gut tissue, and at 4 you have no villi left, and the wall of the small intestine is flat and has a scalloped appearance in folds. The blood test and the intestinal biopsy by endoscopy are the "gold standard" for diagnosing celiac disease. The third step is for the doctor to monitor the results on a gluten free diet. If there is great improvement within six months, then that is taken as confirmation that the person has celiac disease. If you had a negative tTG test, and still think you might have celiac disease or at least a sensitivity to gluten, see the home test for gluten testing under the Gluten Sensitivity section.
from Celiac Disease Blood Tests to What is Celiac Disease
|